Hi Shawna,
I just finished my last pack of pills – how do I get more?
-Anonymous
Good Question!
Prescription and pharmacy questions are some of the most frequently asked questions we get – it’s about time I blog about it.
Before I begin, let me clarify some terms.
Prescriptions: Medications that require a clinician’s approval.
Over the Counter Medications: Medications, like Tylenol or NyQuil, which can be purchased without a clinician’s approval.
Refill: A refill is more of your medicine that you already have a prescription for. Some medicines are only needed once whereas other medicines are needed over a long period of time – like birth control pills.
Pharmacy: Where medications, both prescriptions and over the counter, are dispensed and/or sold. Walgreens, CVS, and Safeway are some of the most common pharmacies used by NGHC patients.

Many places give patients a piece of paper (like the one below) that they must take to a pharmacy in order to get their prescription but here at NGHC we send prescriptions electronically (like an email).

Picking up your prescription:
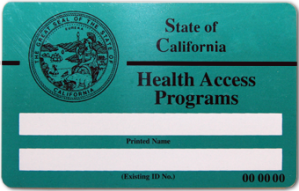
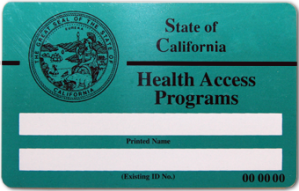
Go to the pharmacy counter and let the pharmacist know you are picking up a prescription. Give them your picture ID (if you have one) and your Family Pact Card. It’s okay if you don’t have an ID because they can verify your identity by asking you various questions (like birth date or address). But it’s really important to have your Family Pact card because it’s the reason the medications we prescribed you are free. Without this card, the pharmacist may attempt to charge you for your medication (which can be very expensive).
*Family Pact does not cover all medications but it does cover the medications we prescribe at NGHC (like birth control and STD treatment). It will not cover the cost of other medication (like acne or asthma medication). If you have any questions about this, ask the person prescribing you the medication or the pharmacist.
If you have any questions about the medication, be sure to ask the pharmacist. Common questions include:
• Should I eat before I take this medication?
• Should I avoid certain food or alcohol when taking this medication?
• How long should I take this medication for?
• Are there any side effects from taking this medication?
It’s really important that you get all your questions answered. Some medications can have some very bad consequences if taken incorrectly.
If you forget to ask the pharmacist or are too embarrassed, you can call NGHC and ask us. We’d be happy to answer any questions about the medication that we prescribed to you.
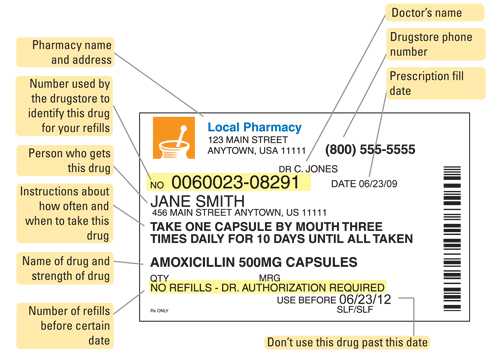
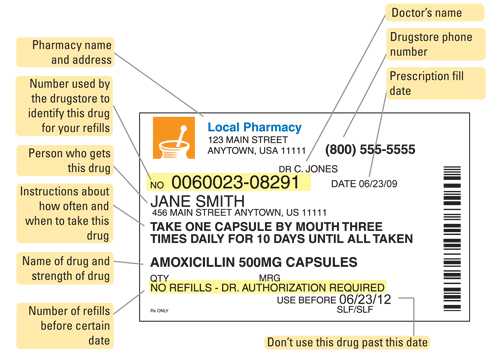
Before you leave the pharmacy, check the label on the prescription and make sure everything is correct. If not, let the pharmacist know. The medication will also likely come with a sheet of information about the medication. Make sure you read it, especially if you have never taken the medication.
The picture below shows you how to read a medication label. All medications will have this information.
Refills:
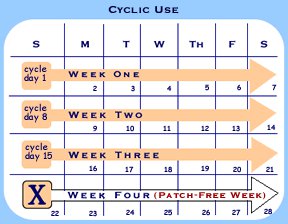
If you are taking a medication more than once, like the birth control pills, you will need refills. For almost every patient we prescribe birth control to, we also give refills. Look at the label and see if you have any refills left. If you do, call the pharmacy BEFORE you run out and ask them to refill the prescription. Be sure to pick it up before you run out.
If the label says you have no refills left, call NGHC and ask for a refill. Whoever takes your call will deliver the message to one of the clinicians so they can send in another prescription for you. It may take a few days for that to happen so make sure you let us know before you are completely out of your medication.
Confidentiality:
All your personal information, including your prescriptions, is confidential. The pharmacy is not allowed to tell anyone, including your parents, about your medications. However, if you use the same pharmacy your family does, we suggest informing the pharmacists that you really do need all your medications confidential. Make sure they have your phone number and know how to contact you if you share your phone number with family.
A few pharmacy tips:
If you use any major pharmacy, like Walgreens or CVS, you can pick up your prescription at any location. You can either walk in or call the location you want to pick them up at and tell them that you normally pick them up elsewhere but that you’d like to get them there. All larger pharmacies are connected and can see where your prescription was sent. Just note, it may take a little longer for your prescription to be ready.
Some major pharmacies have apps that make ordering and refilling super easy. Ask your pharmacy if they have an app.

I hope this answers some of your questions about prescriptions and pharmacies. If you still have questions, let me know (I know this stuff can be a little confusing).
In happiness & health,
Shawna
Reviewed by Kohar Der Simonian, MD